What is Obstructive Sleep Apnea? Understanding the Causes and Solutions
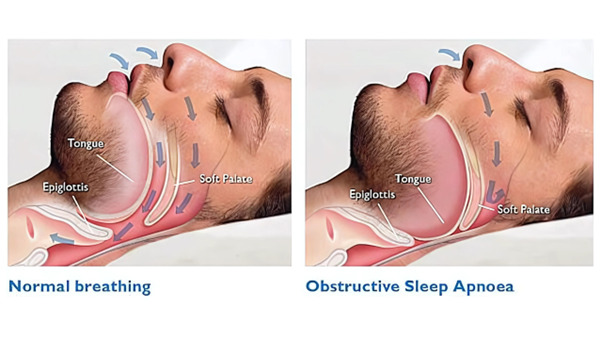
Obstructive Sleep Apnea (OSA) is a common yet serious sleep disorder marked by repeated interruptions in breathing during sleep. This occurs when the upper airways in the nose or throat collapse, causing blocked airflow and disrupted breathing. Each episode of blockage lowers oxygen levels in the body, triggering stress on the heart and leading to frequent awakenings during the night.
OSA affects an estimated 15% of the population, with middle-aged, overweight men being particularly at risk. Factors such as a large tongue, small jaw, or enlarged tonsils can worsen the condition. Left untreated, OSA increases the risk of heart disease, stroke, and other health complications, highlighting the importance of early diagnosis and treatment.
Causes of Obstructive Sleep Apnea
Anatomical Factors
Obstructive Sleep Apnea (OSA) often arises from anatomical issues that obstruct airflow during sleep. Individuals with a small jaw, enlarged tonsils, or a large tongue are more likely to experience airway blockages. These physical traits make it easier for the upper airways to collapse while sleeping, leading to disrupted breathing.
Lifestyle and Health Factors
Excess weight, especially fat deposits in the neck, increases the risk of OSA. Smoking, alcohol consumption, and sedative use further relax airway muscles, worsening symptoms. Maintaining a healthy lifestyle is crucial in managing OSA.
Other Health Conditions
Certain health conditions, like hypothyroidism, can also increase the likelihood of developing OSA. Hormonal imbalances can lead to airway relaxation, further contributing to this sleep disorder.
Symptoms of Obstructive Sleep Apnea
Primary Symptoms
The most noticeable signs of Obstructive Sleep Apnea (OSA) include loud snoring, gasping, or choking during sleep. These episodes occur when the airway becomes blocked, often leading to frequent awakenings and disrupted sleep patterns. If left untreated, these interruptions can severely impact your overall sleep quality.
Secondary Symptoms
OSA doesn’t just affect your nights — it can cause significant daytime issues too. Common symptoms include daytime fatigue, excessive sleepiness, and cognitive difficulties such as trouble concentrating. Many people with OSA also experience morning headaches, which are linked to poor oxygen supply during sleep.
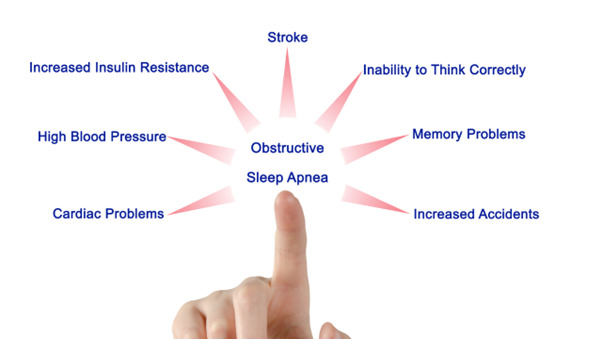
Complications if Untreated
If OSA remains untreated, it can increase the risk of serious health complications, such as high blood pressure, heart disease, and stroke. These risks are due to the strain placed on the heart as a result of reduced oxygen levels during repeated breathing disruptions.
Diagnosis of Obstructive Sleep Apnea

Polysomnography (Sleep Study)
Polysomnography, or a sleep study, is the gold standard for diagnosing Obstructive Sleep Apnea (OSA). This overnight test monitors your breathing, oxygen levels, heart rate, and other vital signs while you sleep. By recording apneic (complete pauses in breathing) and hypopneic (partial reductions in airflow) episodes, doctors can determine the severity of OSA and tailor a treatment plan accordingly.
Physical Examination
In addition to a sleep study, a physical examination helps identify structural causes of OSA. Using a nasendoscope, a flexible camera, ENT specialists examine areas prone to obstruction, such as the nose, soft palate, tonsils, or the base of the tongue. This examination can guide decisions regarding potential surgical interventions.
Treatment Options for Obstructive Sleep Apnea

Conservative Treatments
Lifestyle Changes
Conservative treatments for Obstructive Sleep Apnea (OSA) begin with lifestyle changes. Weight loss can significantly reduce airway obstructions, while sleep hygiene improvements, such as sleeping on your side and avoiding alcohol before bed, help prevent airway collapse during sleep. Positional therapy, like using pillows to keep you from sleeping on your back, can also ease symptoms.
Positive Airway Pressure (PAP) Devices
The most effective treatment for OSA is CPAP (Continuous Positive Airway Pressure), which uses air pressure to keep airways open during sleep. Adaptive ventilation devices, designed for more severe cases, adjust pressure automatically to ensure consistent airflow and are highly effective in reducing OSA events.
Oral Devices
Mandibular Advancement Devices (MAD) reposition the lower jaw during sleep, preventing airway obstruction. This option is suitable for patients with mild to moderate OSA.
Surgical Interventions
In more severe cases, surgical treatments may be considered. Procedures like somnoplasty use radiofrequency to reduce excess tissue in the airway. Tonsillectomy is particularly useful in children with enlarged tonsils, while Uvulopalatopharyngoplasty (UPPP) removes soft tissue to widen the airway. Inspire Upper Airway Stimulation involves a nerve stimulator to keep the airway open during sleep, offering relief for certain patients.
Post-Treatment Considerations and Outcomes
Recovery and Adaptation
After treatment for Obstructive Sleep Apnea (OSA), most patients experience noticeable improvements relatively quickly, especially those using CPAP devices. Relief from symptoms like snoring and interrupted sleep can begin almost immediately, though full recovery may take a few months of consistent treatment.
Long-Term Management
Sustaining improvement depends on long-term management, particularly regular use of prescribed devices like CPAP. Consistency is crucial, as discontinuing treatment may result in the return of symptoms and associated risks. Maintaining healthy lifestyle changes is equally important for ongoing success.
Complications and Side Effects
While effective, CPAP devices may cause discomfort with mask fit, and surgical interventions can have side effects, such as swelling or pain. Most issues are manageable, and healthcare providers can help adjust treatments to ensure better comfort and outcomes.
Conclusion
If you suspect you may have Obstructive Sleep Apnea (OSA), it’s essential to seek medical attention from an ENT specialist. Early diagnosis and treatment can prevent serious long-term complications such as heart disease, stroke, and other health issues. Don’t wait—addressing OSA early can dramatically improve your quality of life.
Treatment for OSA is not a one-size-fits-all approach. Visit https://earnosethroat.com.sg/sleep-apnea-treatment-singapore-sleep-clinic/ today to set up an appointment with experienced ENT doctor to tailor a treatment plan based on your specific causes, symptoms, and severity.
Whether through lifestyle changes, CPAP therapy, or surgery, your journey to better sleep and health should be guided by an ENT specialist for the best outcomes.
Remember, consistent treatment and follow-up are key to managing OSA effectively. With the right care, you can enjoy restful nights and avoid the potential risks associated with untreated sleep apnea. Prioritizing your sleep health is an important step toward a healthier future.