What to Expect From an ENT Exam: A Guide for Patients
Ear, nose, and throat (E.N.T) treatments are specialized procedures used to diagnose and treat a variety of conditions that affect the ears, nose, and throat.
These treatments can range from relatively simple surgical procedures or medications to highly advanced imaging techniques.
By working with an experienced and knowledgeable E.N.T. specialist, you can ensure that your treatment plan is tailored to your individual needs.
Common Causes of Ear, Nose, and Throat Problems
Ear, nose, and throat problems are often caused by infections such as the common cold or flu, allergies to pollens or other airborne particles, and sinusitis.
Other causes of E.N.T. issues can include structural problems such as a deviated septum or polyps, growths in the nasal passages, and tumors in the ears or throat.
In some cases, trauma to the head or neck can also cause ear, nose, and throat problems.
Diagnosing and Treating the Most Common Conditions
E.N.T. specialists use a variety of tests to diagnose E.N.T. problems, including physical examinations, imaging techniques such as X-rays and CT scans, blood testing, and even endoscopy procedures in some cases.
Once a diagnosis is made, treatment can range from lifestyle modifications and to surgery. Depending on the diagnosis and severity of the condition, your E.N.T. specialist will recommend a treatment plan that is best for you.
Potential Side Effects and Risks of Treatment Options
Antibiotics
Antibiotics are commonly prescribed for ear, nose, and throat infections to fight bacterial infections.
However, like all medications, antibiotics come with potential side effects, including, nausea, vomiting, diarrhea, and allergic reactions.
Furthermore, inappropriate use of antibiotics can lead to an increase in antibiotic-resistant bacteria.
Over-the-counter (OTC) remedies
OTC remedies like decongestants and painkillers can be an effective treatment option for mild ear, nose, and throat issues.
However, they can also cause unwanted side effects, such as dizziness, sleep disturbance, and dry mouth.
Nasal steroids
Nasal steroids are a common treatment option for allergic rhinitis (hay fever) and nasal polyps. Although nasal steroids can be highly effective, they can also lead to nasal dryness, nosebleeds, and headaches.

Surgery
Surgery is a treatment option for severe or chronic ear, nose, and throat issues. However, all surgeries come with potential risks, including bleeding, infection, and damage to surrounding tissue or organs.
Radiofrequency Therapy
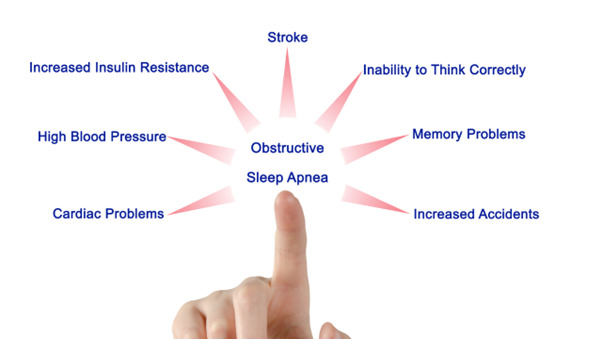
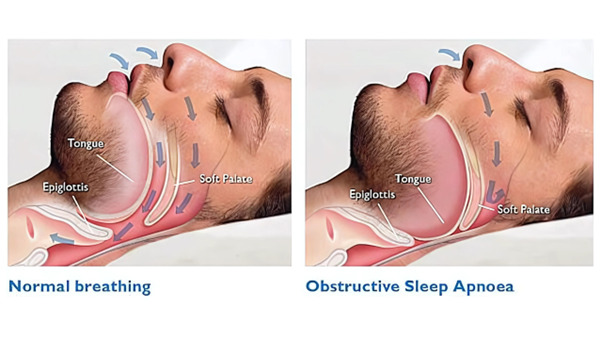
If you suffer from snoring or sleep apnea, radiofrequency therapy may be recommended. While this treatment can help, it can also lead to post-treatment problems, including dry or sore throat, nausea, and swelling.
Chemotherapy
Chemotherapy is typically recommended for advanced cases of throat cancer and can help shrink tumors. However, chemotherapy can have devastating side effects, including nausea, vomiting, hair loss, and fatigue.
Radiation therapy
Radiation therapy, like chemotherapy, is often prescribed for advanced throat cancer. However, this treatment can lead to hoarseness, dry mouth, mouth sores, and hair loss.
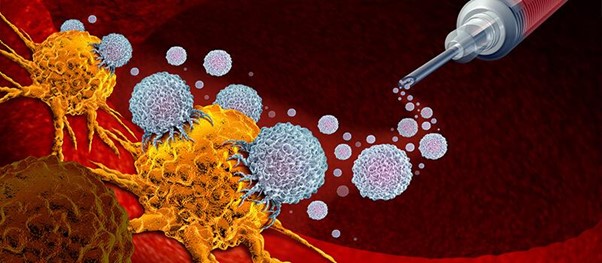
Immunotherapy
Immunotherapy is a relatively new treatment option for advanced cancers. It is designed to provoke the patient’s immune system to target and kill cancer cells. While this method is highly effective in many cases, it can also cause allergic reactions, fever, and chills.
Microdebrider-assisted turbinoplasty
Microdebrider-assisted turbinoplasty is a minimally invasive treatment option for nasal obstruction. However, this procedure can lead to adverse effects like nasal bleeding, scabbing, and congestion.
Laser-assisted uvulopalatoplasty
Laser-assisted uvulopalatoplasty (LAUP) is used to treat snoring and sleep apnea. While this procedure can help in many cases, it can also lead to pain, swelling, and bleeding.
The Latest Developments in Effective E.N.T Techniques
E.N.T. specialists are constantly researching and developing new techniques and treatments for ear, nose, and throat issues, allowing them to provide better results with fewer risks or side effects.
Some of these new techniques include minimally-invasive, robotic-assisted surgery and advanced imaging techniques for diagnosing complex conditions.
Noninvasive E.N.T Care Strategies for Prevention & Maintenance
In addition to treatments for existing ear, nose, and throat problems, many E.N.T. specialists also offer preventive and maintenance care to help keep your ears, nose, and throat healthy.
These strategies can include eating a balanced diet, avoiding exposure to potential irritants, quitting smoking, and getting regular check-ups with your E.N.T. specialist.

FAQs about Ear, Nose & Throat Care
Q: How often should I get checked by an E.N.T. specialist?
A: Depending on your individual risk factors, your E.N.T. specialist may recommend that you have a yearly check-up or more frequent visits if necessary.
It is important to follow their recommendations and schedule regular appointments to keep your ears, nose, and throat healthy.
Q: What are the benefits of seeing a specialist for E.N.T care?
A: An experienced E.N.T. specialist can provide expert diagnosis and treatment for ear, nose, and throat conditions, which can result in fewer complications and improved results.
In addition, they can provide preventive care strategies to help you maintain optimal ear, nose, and throat health.
Q: Are there any risks associated with E.N.T treatments?
A: As with any type of medical treatment, there are potential risks or side effects associated with certain E.N.T. treatments such as surgery or medications.
Be sure to discuss these with your E.N.T. specialist before beginning any treatment plan.
Conclusion
By working closely with an experienced and knowledgeable E.N.T. specialist, you can ensure that your ear, nose, and throat care is tailored to your individual needs and get the best possible outcome from any treatments or preventive strategies recommended.
If you are experiencing any issues with your ears, nose, or throat, be sure to contact your E.N.T. specialist to schedule an appointment.
Learn more.